- Written:
- Author: Edward
- Posted in: exosomes, News
- Tags: arthroscopy, bankhart tear, exosomes, hip, joint cartilage, knee, labrum, meniscus, shoulder dislocation, slap lesion
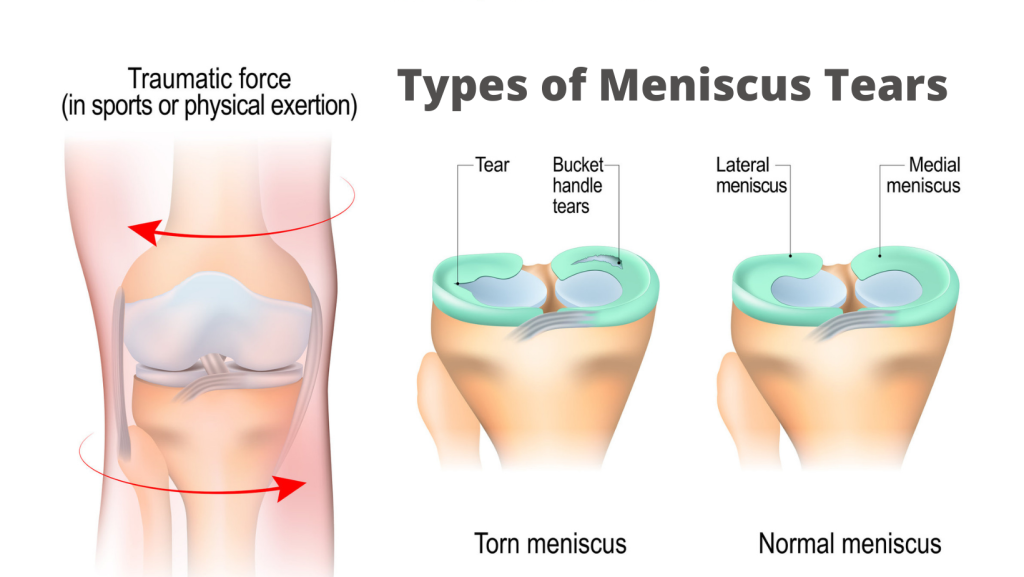
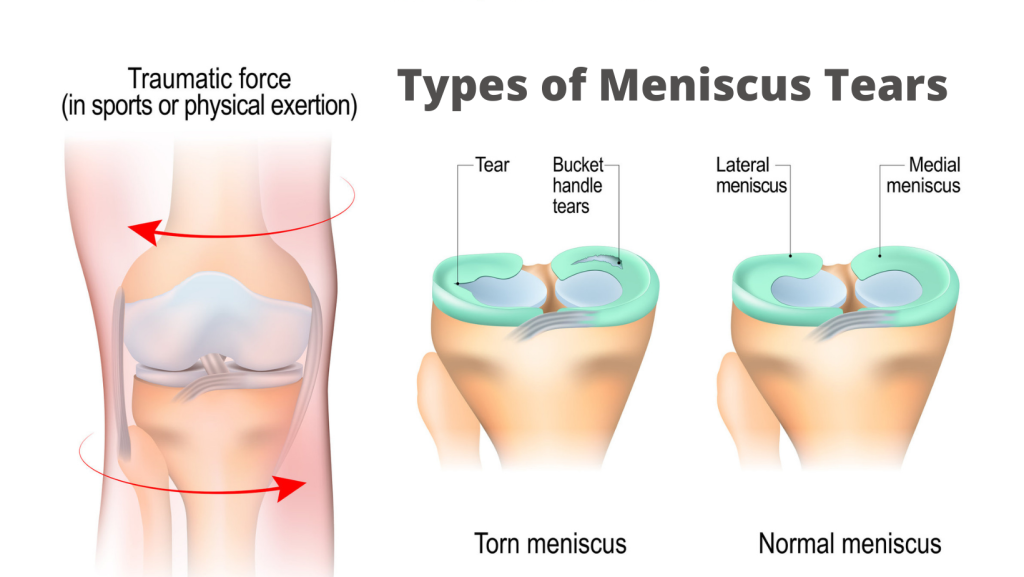
This weekend, I am in New York City seeing a couple of patients and visiting with my two sons, who now live in the East Village. About 10 weeks ago, my 20-yo was goofing around with his girlfriend (getting a piggy back ride) although he weighs twice as much as her. He fell on a twisted foot and immediately experienced knee pain that was severe, limiting his ability to flex the knee. There was mild clicking and the pain was worsened while twisting on the single leg. There is only one thing this could be: a torn meniscus.
Six weeks ago, at my older son’s Cornell graduation (and five weeks after the initial injury), I treated my son’s knee joint, hoping the meniscal cartilage would heal. Yesterday, even though I brought an extra vial to retreat his knee, he said it felt almost normal, didn’t hurt, and had no limited range of motion. He wanted to start running again but I told him to wait another two weeks so that it would be 8 weeks from treatment because the new cartilage is often disorganized Type 3, not permanent Type 1 cartilage and can be reinjured easily.
Strike while the iron is hot
AS a part of being alive, we are constantly becoming injured and repairing. In the case of muscles, it makes them stronger to rebuild. In the case of tendons and cartilage, they appear to repair to nearly 100% but if you reinjure them too frequently, the stem cells in the cartilage might not have the time to restore their telomeres between cell divisions and they undergo replicating senescence (aging from copying).
The awful truth of getting old is that throughout our bodies, we acquire injuries but the local stem cells got over-copied and are now unable to reproduce but they are not dying and being replaced by younger ones. That is what creates tendinosis and arthrosis.
In my clinical experiences, from my self-treated right knee meniscus four years ago to yesterday’s non-treatment of my son, it is clear that treating recent injury is more effective than old injury. When I say “strike while the iron is hot” I mean that the acute inflammation of a recent injury brings in immune cells and increased blood flow that makes the repair more efficient.
I’ll never forget a woman in her 40s who fell from a horse, breaking her vertebrae on five segments. She was in a lot of pain and I suggested epidural injection. She was scared and instead took IV and sure enough, because of the local inflammation, the exosomes went exactly where they were needed and within two weeks, she was totally pain free and working out in the gym
Shoulder and hip Labra
Cartilage lining the inside of joints are very similar. Because of aging, weakening, microtears, trauma, and poor alignment, we can get tears in the shoulder cartilage (such as the biceps tendon causing a SLAP tear or a dislocation causing a Bankhart tear). In the hip, the lining cartilage is also called labral and gets torn as well. Since those two joints are easily accessible with a simple office procedure, I recommend early treatment in the case of injury although we do see improvement even years after initial injury (as with the case of my own meniscus)
I was just texting a 36-yo patient who I did a shoulder injection nine days ago for a Bankhart tear to the labrum and a fracture to part of the shoulder socket 25 days ago after falling on an outstretched hand. The key part of his story is that this 36yo man had a 70yo shoulder from injury as a lacrosse player when he was younger. It appears that the exosome injection is accelerating his normal repair according to his physical therapists and his subjective account.
“It’s feeling great and I went to my first PT on Friday and they were shocked [at] how quickly I’m recovering and the mobility and strength I have already.”
The third option!
In standard practice there are two options to treat torn joint cartilage in joints: one is to do arthroscopy and re-anchor/sew/resect the moving and damaged tissue- or wait.
While we wait, there is inflammation but as I explained above, it is often too little and too late. The inflammation brings a natural “prolotherapy” by recruiting stem cells, which secrete their exosomes, but the result is incomplete repair and aging of the local cartilage-producing stem cells. This sets you up for more damage and arthritis in the future.
Now, I believe there is a third option. After injury, instead of getting 100% of the exosomes your old and damaged body can produce to stimulate new blood vessels, dedifferentiation, stem cell migration, you can now get thousands of times the exosomes you could naturally make by simply having us inject them.
To learn more about shoulders and knees, watch these videos.


1 thought on “Torn joint cartilage”
fantastic! timing is everything